Indicators of the collapse of Lebanon's healthcare system are worsening, with preventable diseases spreading widely and at an accelerating pace. Lebanon is witnessing a surge in cases of cholera, hepatitis A, measles, and meningitis, diseases exacerbated by the Israeli aggression on Lebanon and the ongoing economic collapse since 2019. Decades of austerity and a healthcare system based on excessive privatisation have weakened public health services, rendering them incapable of containing these outbreaks, leading to an unprecedented acceleration of the health crisis.
In 2025, Lebanon faces the risk of public health deterioration unless these risks are urgently prioritised. A combination of interconnected factors—war, declining living standards, continuous inflation, and deteriorating infrastructure—has created ideal conditions for epidemics to thrive, compounded by rampant malnutrition and limited access to healthcare services.
The report "Lebanon Crisis, Risk Analysis 2025," prepared by Save the Children in collaboration with Data Friendly Space in the last month of the previous year, assesses the likelihood and impact of expected risks in Lebanon for 2025. The findings indicate a high probability of cholera, hepatitis A, measles, and meningitis outbreaks, with signs of spread already evident, exacerbated by mass displacement during the war and the near-total collapse of essential services. The potential for these epidemics poses a grave danger, with over 1.2 million people in urgent need of food assistance, as malnutrition further increases the population's vulnerability to disease. Meanwhile, Lebanon's healthcare system, already strained by conflict and austerity policies, is buckling under the weight of accumulating health crises, chronic underfunding, and the absence of a clear public health vision.
These risks reflect deep structural deficiencies in Lebanon's system, which have prioritised the interests of financial and commercial elites over public health. This policy has intensified since the 2019 economic crisis. The question today is no longer whether Lebanon will face health crises but how devastating they will be and whether they will become tools for imposing further structural violence on the most vulnerable populations.
Cholera: A Symbol of Structural Failure
The resurgence of cholera, a disease linked to contaminated drinking water and poor sanitation, has struck Lebanon with alarming force. In the 2022 outbreak, 8,007 suspected cases were recorded, including 671 confirmed cases and 23 deaths. The situation is expected to worsen, as over 36 water facilities were damaged by Israeli attacks, leaving more than 400,000 people without access to safe drinking water source. This potential crisis is not only a result of infrastructure collapse, but also reflects deeper political factors. Water and sanitation services have eroded due to decades of underinvestment and neglect. The state's inability—or unwillingness—to provide basic services to residents or engage seriously in reconstruction efforts has forced millions to rely on fragmented and insufficient humanitarian aid, which faces funding shortages that may worsen with the halt of U.S. assistance.
The concern is not just the possibility of a new cholera outbreak—especially since the 2022 outbreak was successfully contained—but the sustainability of the risk, suggesting that cholera could become endemic in Lebanese society after being eradicated in the 1990s.
Hepatitis A: A Sanitation Crisis
Hepatitis A, a viral liver infection, has seen a sharp rise in cases, with 2,086 reported in early 2024 compared to just 609 in 2022. The virus spreads through contaminated food and water and thrives amid Lebanon's deteriorating sanitation conditions. Unlike measles or meningitis, there is no national vaccination program for hepatitis A in Lebanon, making displaced populations in vulnerable areas particularly susceptible to severe infection.
A similar or larger outbreak is expected in 2025, especially in southern regions where Israeli attacks on healthcare infrastructure have severely reduced access to medical services.
Measles: A Collapsed Vaccination System
Measles, one of the most infectious diseases in human history, has reemerged as a health concern this year. Vaccination rates in Lebanon have collapsed due to the healthcare system's breakdown. According to the World Health Organization, vaccination rates have dropped by 40%, with only 73% of the population receiving a single dose of the measles vaccine and 53% receiving two. Last year alone, 84 confirmed cases were recorded. Given that measles has a basic reproduction number (R0) of 12 to 18—meaning each infection can spread to at least 12 people—the outbreak is expected to worsen unless large-scale vaccination campaigns resume.
Measles disproportionately affects children, especially those under five or suffering from malnutrition. Lebanon's economic collapse has reduced access to food, with over a million people in need of food assistance. Malnourished children face a much higher risk of severe complications from measles, such as pneumonia and encephalitis, a phenomenon well-documented in Gaza. The virus can also erase immune memory, leaving children vulnerable to infectious diseases they were previously vaccinated against.
Meningitis: The Silent Killer
Lebanon recorded 295 meningitis cases in 2024, with the disease spreading rapidly in collective shelters. Meningitis causes inflammation of the protective membranes around the brain and spinal cord and can be fatal if not treated promptly. Key factors behind its spread include overcrowding, poor sanitation, and limited access to healthcare—conditions that have worsened significantly as a result of war and economic collapse.
Newborns and the elderly are most at risk, with their vulnerability increasing due to disrupted vaccination campaigns.
The Erosion of Lebanon's Healthcare System
Lebanon's health collapse is not limited to disease outbreaks but also includes the imminent breakdown of healthcare infrastructure. Over 40 hospitals have been severely disrupted, and 98 primary healthcare centres have closed due to Israeli aggression. Meanwhile, UNRWA, the main provider of healthcare services to Palestinian refugees, faces significant funding cuts, further limiting access to care for one of Lebanon's most marginalised groups. The recent U.S. decision to freeze aid is also expected to lead to sharp reductions in the budgets of UN agencies and NGOs providing humanitarian health assistance in Lebanon.
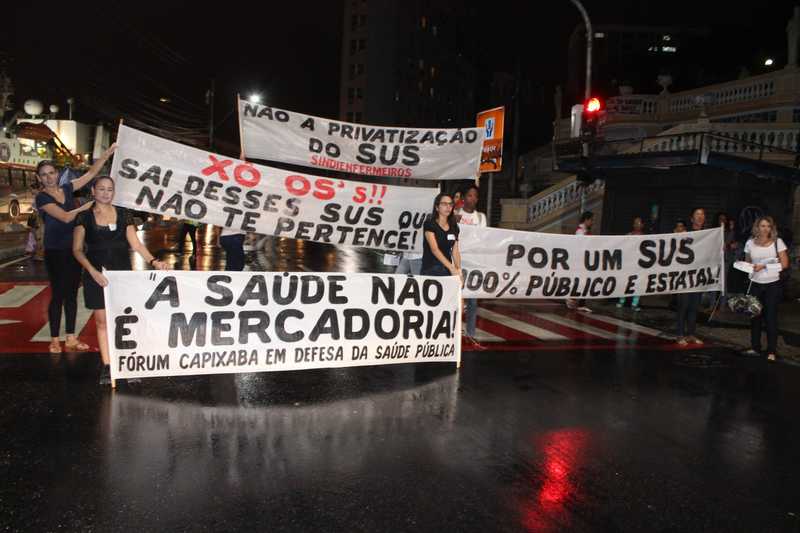
The collapse of the healthcare system was not solely a direct result of the recent war but also the outcome of decades of economic policies that drained public services of their resources and increased their fragility. Mobilising the private healthcare sector to respond to public health crises without the profit incentives that are unavailable today is challenging. The state's reliance on humanitarian organizations to shoulder the responsibility of healthcare delivery has long been criticised, as it exposes Lebanon's healthcare system to the risks of fluctuating foreign funding, a situation evident today with the decline in international aid.
Mental Health: The Neglected Crisis
Amid the physical health crises, Lebanon faces a silent epidemic of mental health disorders. The trauma of war, displacement, and economic deprivation has led to rising rates of anxiety, depression, and post-traumatic stress disorder, particularly among children and women. The prospects of ongoing violence and prolonged displacement further exacerbate depression and anxiety. With the decline in humanitarian health services, psychological support is nearly non-existent for those who need it most. At the same time, the social stigma associated with mental health disorders prevents many from seeking help, intensifying the crisis.
The Role of Malnutrition and Food Insecurity
The growing food crisis worsens Lebanon's public health crisis. Over a million people are in urgent need of food assistance, while child malnutrition rates have reached alarming levels, with 16.5% of children under five suffering from stunting and 6.6% from wasting. Malnutrition rates among children under five in Syrian refugee camps rise to 25.8%, with even higher rates recorded in northern Lebanon and the Bekaa Valley. The consequences of malnutrition extend beyond increasing the risk of infectious diseases, leading to long-term disabilities such as developmental delays and weakened immune systems.
Water and Sanitation
Lebanon's water crisis is a source of escalating public health disasters. The destruction of infrastructure, lack of investment, and collapse of municipal services have deprived entire communities of access to clean water. With Israel's destruction of 36 major water facilities, over 400,000 people now depend on emergency water distribution programs, which suffer from severe funding shortages and are at risk of being halted at any moment.
Avoiding Further Decline
The year 2025 is likely to mark a new phase in the deterioration of Lebanon's healthcare system to a more primitive level. The Lebanese government's responses to the collapse of healthcare services following the 2019 crisis, the COVID-19 pandemic in 2020 and 2021, the cholera outbreak in 2022, and the neglect of Syrian refugee health have only bought time and temporarily mitigated the effects of the healthcare system's decline. However, they have failed to address the structural causes that continue to push the health of Lebanese society further into decline. The policy of denying crises and shifting the responsibility of response to humanitarian organisations has brought us to this point. Refusing to address the structural factors driving these crises not only revives historical health threats, such as outbreaks of preventable infectious diseases, but also entrenches the impact of overlapping crises. The deterioration of healthcare access, malnutrition, and the collapse of infrastructure create an environment conducive to repeated outbreaks that become increasingly difficult to control over time.
Lebanon is rapidly descending to the level of healthcare systems in low-income countries. Reversing this trajectory requires radical reforms across the entire healthcare system and a comprehensive restructuring of public health policies.
Image : IBRAHIM CHALHOUB / AFP via Getty Images