This is the third in a multiple-part series of studies on CoronaShock. It is based on research by Ana Maldonado (Frente Francisco de Miranda, Venezuela), Manolo de los Santos (researcher with Tricontinental: Institute for Social Research), Subin Dennis (researcher with Tricontinental: Institute for Social Research), and Vijay Prashad (director of Tricontinental: Institute for Social Research). This report was first published by Tricontinental. You can also read the report and download a PDF here.
Friedrich Engels once said: ‘Bourgeois society stands at the crossroads, either transition to socialism or regression into barbarism’. What does ‘regression into barbarism’ mean to our lofty European civilisation? Until now, we have all probably read and repeated these words thoughtlessly, without suspecting their fearsome seriousness. A look around us at this moment shows what the regression of bourgeois society into barbarism means. This world war is a regression into barbarism. The triumph of imperialism leads to the annihilation of civilisation. At first, this happens sporadically for the duration of a modern war, but then when the period of unlimited wars begins it progresses toward its inevitable consequences. Today, we face the choice exactly as Friedrich Engels foresaw it a generation ago: either the triumph of imperialism and the collapse of all civilization as in ancient Rome, depopulation, desolation, degeneration – a great cemetery. Or the victory of socialism, that means the conscious active struggle of the international proletariat against imperialism and its method of war. This is a dilemma of world history, an either/or; the scales are wavering before the decision of the class-conscious proletariat. The future of civilisation and humanity depends on whether or not the proletariat resolves to throw its revolutionary broadsword into the scales. In this war imperialism has won. Its bloody sword of genocide has brutally tilted the scale toward the abyss of misery. The only compensation for all the misery and all the shame would be if we learn from the war how the proletariat can seize mastery of its own destiny and escape the role of the lackey to the ruling classes.
Rosa Luxemburg, The Crisis of German Social Democracy, 1915.
![]()
Ở nhà là yêu nước! (‘To stay at home is to love your country!’), Vietnam, 2020.
Hiep Le Duc
In late December 2019, the Wuhan Centre for Disease Control and Prevention (CDC) in central China’s Hubei Province detected cases of pneumonia of an unknown cause. In the first few days of January 2020, Chinese authorities were regularly informing the World Health Organisation (WHO) as well as other major countries and regions with close ties to China’s mainland, such as Hong Kong, Macao, and Taiwan about the outbreak. On 5 January, the WHO released its first briefing on a ‘pneumonia of unknown cause’ in Wuhan. Little was known about the virus, neither how to properly understand it nor whether transmission could occur between humans. The genome sequence for the novel coronavirus (SARS-CoV-2) was published by the Global Initiative on Sharing All Influenza Data (GISAID) on 12 January. Dr. Zhong Nanshan, a leading Chinese pulmonologist who is advising the Chinese government on this pandemic, confirmed human-to-human transmission of the novel coronavirus on 20 January.
As soon as it was clear that this virus could be transmitted between humans, the Chinese authorities acted. Wuhan, a city of 11 million people, was shut down, the scientific establishment in China – and its collaborators around the world – went to work to understand the virus and the disease (COVID-19), and medical personnel in China rushed to be trained and to help break the chain of the infection. Inside Wuhan, the neighbourhood committees, which include members of a range of other associations, Communist Party cadres, and volunteers of all kinds, hastened to assist with temperature checks, food and medicine distribution, and assistance in hospitals. After ten weeks in lockdown, Wuhan opened once more on 8 April. On 15 May, the authorities started to test all the residents of Wuhan once again in order to protect public health and to resume social and economic activities (China shared the results of this test to aid with studies on the feasibility of the herd immunity theory).
On 30 January, WHO Director-General Dr. Tedros Adhanom Ghebreyesus declared that the outbreak constitutes a Public Health Emergency of International Concern (PHEIC). From its Geneva headquarters, the WHO sent up a flare which effectively read: a highly contagious virus has been detected that requires stringent measures of tests, physical distance, and aggressive sanitation.
At this point, in the aftermath of 20 January, a gulf opened between the capitalist states and the socialist states. Our analysis shows four main areas of differentiation between the socialist and capitalist approach to the virus. The socialist approach is based on:
- Science-based government action
- Public sector production of essential materials
- Public action mobilised to facilitate social life
- Internationalism
In the capitalist states (such as the United States, Brazil, and India), the governments have instead operated in a hallucinatory manner, pretending that the virus is either not real or not contagious and hoping that some extraneous factor would protect their citizens from its dangers. For-profit sector firms have failed to provide the necessary equipment, while public action has been hard to galvanise in atomised societies that lack the habit of organisation and struggle. Finally, to cover up their incompetence, the ruling political class in these states has resorted to stigmatisation and jingoism, using – in this case – the lethal combination of racism and anti-communism to blame China.
In this report, we look at three countries (Cuba, Venezuela, and Vietnam) as well as one state (Kerala, India) to investigate how these socialist parts of the world have been able to handle the virus more effectively.
Cuba
On 17 January, Cuban media reported the detection of a mysterious pneumonia in China that, at that point, had killed two people and infected forty-one. When more information came in about the novel coronavirus, the government began to disseminate the WHO’s reports. The Cuban media provided comprehensive coverage of the decisions made in China to implement lockdowns and other measures to break the chain of the infection. On 28 February, Miguel Díaz-Canel Bermúdez, President of Cuba, spoke by phone with Xi Jinping, President of China. During the call, Díaz-Canel expressed the firm support and solidarity of the Cuban people, their government, and the Communist Party with China’s struggle against the virus. Cuba offered to help in any way it could to assist the Chinese people. BioCubaFarma, a public sector firm, increased its production of Interferon Alpha 2B and, as of 24 February, had provided more than 150,000 double dose vials of the drug to China.
On 28 January, Dr. José Ángel Portal Miranda, head of the Ministry of Public Health (MINSAP), convened a national-level meeting on the novel coronavirus. Medical vigilance was to be the priority, which is why the government created a National Working Group (NWG) to lead the struggle. MINSAP began to train all public health personnel – over 95,000 doctors and 84,000 nurses – to diagnose and treat cases of COVID-19. A public campaign began to call for vigilance of symptoms and heightened hygiene. Media platforms shared this information, but so did mass organizations such as the Federation of Cuban Women (FMC), the Committees for the Defence of the Revolution (CDRs), and the Federation of University Students (FEU). Dr. Francisco Durán García, the national director of epidemiology of MINSAP, made the first official statement that day. He calmly explained that the administration had designed a plan ‘similar to the plan we developed when the Ebola epidemic hit several countries’. Dr. Carmelo Trujillo Machado, national head of the MINSAP International Health Control Program, said that officials would be vigilant at ports of entry for travellers with any known symptoms of COVID-19.
The National Working Group authorised the immediate purchase of protective gear, medical equipment, and reactive agents. The production of thirty critical medical products became a priority. Agencies in Cuba began a renewed emphasis on the research and development of candidate vaccines and anti-viral treatments to be shared with China. By April, the Centre for Genetic Engineering and Biotechnology (CIGB) started the first clinical trials on a vaccine that could boost the immune system. Dr. Gerardo E. Guillén Nieto, the director of Biomedical Research at the China-Cuba Centre for Biotechnological Innovation (CCBJIC) in Hunan, China said that his team was examining whether the innate immune system could be activated and, if activated, would produce a specific immunity against the virus. There are no specific vaccines for this disease, but Cuba, he says, ‘has products that already exist’.
On 10 March, four tourists who had arrived from Lombardy (Italy) showed symptoms of COVID-19. When they tested positive for COVID-19, they were shifted to the Pedro Kouri Institute of Tropical Medicine (IPK), which has a long history of combatting epidemics. The IPK, along with regional hospitals in Santa Clara and Santiago de Cuba, was designated as the primary site for testing patients suspected of having COVID-19. Each of these hospitals has the capacity to test 1,000 patients per day. The government decided to place all travellers arriving in Cuba under fourteen days of medical observation.
On 17 March, 28,000 students from Cuba’s thirteen medical universities joined a campaign to visit every home in the country. The students went to check each person for symptoms, and if they found someone with symptoms, they referred them to their community’s family doctor. This doctor would then make a decision about whether or not to test the person. Within a week, the medical students had visited six million Cubans – half of the island’s population. With this approach, close to 40,000 people were tested for COVID-19 by 26 April. In the province of Villa Clara, the students visited 250,000 people, leading to the detection of 2,687 cases with respiratory symptoms, including five potential COVID-19 cases most likely to test positive. Thousands more foreign medical students on scholarships provided by Cuba joined this campaign. Ishaira Nieto Rosas, a third year student from Puerto Rico, said that for foreign students these visits were voluntary, but ‘in these moments you realise that our work is very important and that the population is aware of that. It does not matter how many doors we have to knock on, or how many times we have to shout good morning. We do this because the country needs us, and we do it with great pride’.
On 20 March, President Díaz-Canel, along with seven members of Cuba’s Council of Ministers, went on television to report on the steps taken thus far and to outline further measures. ‘We have a responsibility to protect human lives and the entire social fabric’, he said, ‘with serenity, realism, and objectivity. There can be neither panic nor overconfidence’. A science-based attitude defined Cuba’s response. By that date, 21 people had tested positive for COVID-19 and another 716 people were under observation in hospitals. The government put forward several measures:
- Cuban nationals who returned home from abroad would be placed under a fourteen-day quarantine.
- Sixty thousand tourists would leave the country; the entry of travellers would be heavily regulated, which would impact tourism, one of Cuba’s key sources of revenue.
- Physical distancing was mandated.
- People vulnerable to the virus and those who were not working in key industries were mandated to self-quarantine at home.
- The Ministry of Internal Commerce suspended all public activities. Food stores and farmers’ markets would be kept open under the strictest health regulations. Restaurants could remain open but only at 50% capacity.
- Minister of Labour and Social Security Marta Elena Feitó Cabrera said that ‘No one will be left helpless’, and measures were implemented to ensure this. Tax payments for self-employed private sector workers were suspended. For the first month of the quarantine, furloughed workers received 100% of their salaries; after that, workers were promised 60% of their salaries. Workers in the private sector were told that they would receive the equivalent of the national minimum wage.
- To stave off the possibility of hunger, the Cuban authorities expanded the existing rationing system in order to guarantee each family equitable access to food and basic sanitation supplies during the pandemic. Ration cards were used for distribution through 12,767 neighbourhood stores; these cards offer a basic food basket that includes cooking oil, sugar, rice, and beans, and was expanded to include eggs, potatoes, vegetables, an extra pound of chicken per person, and extra soap, toothpaste, and bleach. Despite its limitations, the ration cards and neighbourhood stores have served 3,809,000 families and limited price gouging.
By 6 April, the number of confirmed patients rose to 396, with 1,752 hospitalised. The government announced additional measures based on the national plan. These included suspending all non-essential economic activities, sit-down service in restaurants (only pick-ups and deliveries allowed), urban public transportation, and postponing payment for water, electricity, and gas.
The backbone of Cuba’s response to COVID-19, as in other socialist countries, has been public action. The Committees for the Defence of the Revolution (CDRs), founded in 1960 under the threat of a possible US invasion, have an estimated 8 million members (out of a population of 11.34 million). The committees are organised on a block-by-block basis; they mobilise the people to help the most vulnerable in each community, to participate in health campaigns, and to provide food and shelter during the hurricane season. In the eastern city of Santiago de Cuba, CDR members like Juana Guerra, a university professor and a member of the Federation of Cuban Women, made 16,000 masks. Members of the Federation of University Students volunteer in different cities, helping to clean and cook in isolation centres, delivering supplies to families under quarantine, and working in designated support centres preparing food for medical personnel and vulnerable families. Inspired by the battles of the past, many students proudly say that COVID-19 has become their Bay of Pigs (#EsteEsMiGiron).
Internationalism is at the core of the revolutionary Cuban ethos. In 2005, Cuba founded the Henry Reeve International Medical Brigade to provide emergency health assistance around the world; since then, it has sent twenty-five contingents abroad, aiding 3.5 million people in twenty-three countries. This brigade is now at the centre of the fight against COVID-19, responding to requests to send Cuban health workers to countries around the world. On 15 March, the first contingent of 130 epidemiologists and other medical specialists left for Venezuela. Since then, thirty-three more contingents made up of 3,337 health workers have gone to work in twenty-seven countries in Europe, Africa, and Latin America (the contingents range from two doctors in Grenada to 217 health workers in South Africa). Many of these countries have come under increased pressure from the US government to deny Cuba’s help. US Secretary of State Mike Pompeo has led the charge, accusing the island of profiting from the pandemic. Cuba’s foreign minister Bruno Rodríguez Parrilla responded to the US smear campaign, saying, ‘What right does the Secretary of State have to put pressure on sovereign governments to deprive their nation[s] of medical care?’
As the world entered into CoronaShock, the British cruise ship MS Braemar was left stranded in the Caribbean carrying 682 passengers, including five with COVID-19, desperately looking for a port in which to dock. While other countries refused to allow the ship to dock, Cuba – at significant risk – opened its doors and organised the disembarkment and return home of its passengers, stating that ‘These times call for solidarity, understanding health as a human right and strengthening international cooperation in order to address our common challenges; i.e., values that are inherent to the humanist practice of the Cuban Revolution and people’.
Cuba’s revolutionary system has given it the strength and ability to survive in the face of blockades and pandemics, integrating workers, peasants, scientists, mass organisations, and civil defence systems with a party and a government that puts human life at the centre of its attention.
![]()
We sent a doctor to Cuba; the doctor transformed into millions, 2020. #CubaSavesLives
Vietnam
On 16 January, before it was clear that the new virus could be transmitted between humans, Vietnam’s Ministry of Health informed the other government agencies and the public about the dangerous virus and urged immediate action. Five days later, on 21 January, the Ministry of Health gave detailed instructions to hospitals and clinics about how to tackle the virus. On 24 January, Deputy Health Minister Đỗ Xuân Tuyên said that inspections would take place at all border posts; this was an important decision, since Vietnam shares a 1,400-kilometre border with China, and this border is only a ten-hour bus ride from Wuhan. On 30 January, the Vietnamese government – led by Prime Minister Nguyễn Xuân Phúc – established a national steering committee on epidemic prevention. Two days later, on 1 February, Prime Minister Nguyễn declared what was effectively a national emergency.
The Communist Party of Vietnam very early on offered a motto: ‘fighting the epidemic is like fighting against the enemy’. But this fight was to be conducted with a scientific attitude. Testing began at the border points, and epidemic control teams began to test the population and carry out contact tracing if an infected person was identified. The National Institute of Hygiene and Epidemiology was able to create a test very quickly, which was used extensively in the country; over 100 laboratories across the country performed real-time polymerase chain reaction (PCR) testing, which allowed for much faster COVID-19 results at the rate of 27,000 samples per day. On 10 March, the government released the NCOVI mobile application to facilitate contact tracing. Rather than lock down the entire population, the epidemic teams studied the population and isolated and treated those with symptoms, those who tested positive for COVID-19, and anyone who they came into contact with; any region with particularly high numbers was quarantined.
Based on the scientific knowledge available, the Vietnamese authorities followed a four-tier approach to isolation:
- Tier one: anyone with a confirmed diagnosis is isolated in a health facility (in these cases, self-quarantine is not permitted).
- Tier two: anyone with close contact with the confirmed cases must be tested and go into a government-run quarantine centre.
- Tier three: anyone who has been in close contact with the people in tier two must self-isolate at home.
- Tier four: if there is a particularly bad outbreak in a village or a hospital, the entire village and hospital must go into lockdown.
This multi-tier isolation system helped the authorities break the chain of infection. But the government remained vigilant. On 30 March, soon after the Bach Mai Hospital in Hanoi – which had been essential in the fight to break the chain – experienced a flare of cases, the government announced a national pandemic.
The Ministry of Health posted a music video to explain the concept of physical distancing and hand washing; this video went viral on Tik Tok, where young people created a dance to go with it. The message was broadcast within days. Telecommunications firms – including private companies – sent three billion messages about COVID-19 to those with mobile phones. Masks were mandated in public and alcohol-based hand sanitisers were distributed and made available for sale everywhere. Schools and religious sites were all immediately closed.
The government directed public sector units to produce necessary equipment, including Personal Protective Equipment (PPE) and ventilators, as well as hand sanitizer and medicines. There was enough industrial capacity that could be directed to produce these goods without any concerns about price gouging, since these are public sector enterprises. On 8 April, the government of Vietnam sent 450,000 units of PPE to the United States in an act of solidarity. This is the same country which was bombed beyond belief by the United States government, which used such harsh chemical weapons that the people remain scarred by. Vietnam’s agriculture will not recover for generations.
The private sector followed suit, and so did philanthropists who set up ‘Rice ATMs’ to distribute food to those who had lost their incomes. The government set up food kitchens to feed any one in need.
Vietnam, with a population of 100 million, has had no fatalities from COVID-19 as of early July.
![]()
Cảm ơn Việt Nam! (‘Thank you, Vietnam!’), Vietnam, 2020.
Hiep Le Duc
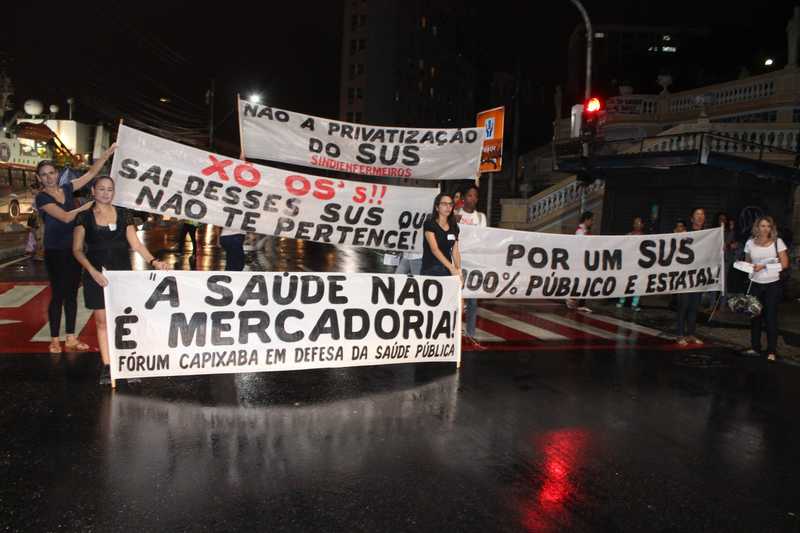
Venezuela
On 26 February, Brazilian authorities reported the first case of coronavirus; this case was also the first to be reported in Latin America. Two days later, on 28 February, the Venezuelan government created the Presidential Commission for the Prevention and Control of Coronavirus (weeks before the first case was reported in the country on 13 March). Strikingly, during the same time frame, the United States government decided to deepen its hybrid war against Venezuela – despite the highly contagious nature of the coronavirus, and despite the warnings of the WHO.
Before the pandemic, Venezuela had already been under severe US sanctions, putting pressure on Venezuela’s economy as a whole and sabotaging Venezuela’s public health system. In 2018, the Venezuelan Pharmaceutical Federation reported 85% shortages of essential medicines. Another study from 2018 showed that 300,000 people are at risk of dying because they lack access to key medicines for HIV, kidney disease, cancer, and diabetes as a result of the sanctions. Venezuela turned to its international allies – China, Cuba, Iran, and Russia – to provide necessary equipment and support. Squeezed by the hostile US-driven sanctions regime and by a blockade by US warships, the Venezuelan government and its allies demonstrated nerves of steel in their decision to break the US embargo.
On 13 March, Venezuela’s Vice President Delcy Rodríguez confirmed the first positive cases of COVID-19: a forty-one-year-old woman returning from travels in the European Union and the United States and a fifty-two-year-old man returning from Spain. The previous day, the government had suspended flights – effective 15 March – from Europe, Colombia, Panama, and the Dominican Republic and began checking for symptoms at airports and seaports. Because of the cases of the travellers returning from Spain, mandatory quarantines were ordered for all passengers who arrived on Iberia flight 6673 on 5 and 8 March.
The government took the WHO advisories seriously and banned all public gatherings, suspended all schools, ordered the use of face masks on public transportation, and, on 15 March called for a total quarantine in certain states of the country (La Guaira, Miranda, Zulia, Apure, Táchira and Cojedes, as well as in the city of Caracas). Within two days, the government confirmed sixteen new cases, and so it extended the quarantine to the entire nation for one month. The use of face masks in public was declared compulsory.
It was imperative, again based on the advice of the WHO, to collect relevant medical and epidemiological information about the population. On 16 March, the government announced that the Sistema Patria (‘System of the Homeland’) – the national card system established by President Nicolás Maduro in 2016 to facilitate access to social programs and electronic payments – would be used as an instrument in the fight against the disease. In 2017, Maduro’s administration established this web-based platform as a way to reach the most vulnerable parts of the population in the fight against sanctions-induced problems. Through a voluntary registration process, over eighteen million of Venezuela’s roughly twenty-eight million residents enrolled in the system, making it the most comprehensive way both to collect information and to deliver goods and services to the people. Over the years, the Sistema Patria has become the basis for organising the food supply, allocating monetary assistance, and experimenting with digital currency. In the case of the struggle against COVID-19, the system has been used to deliver cash assistance to the people as well as to do a proper inventory of the people’s medical needs.
On 26 March, the US Department of Justice accused the Venezuelan leadership of drug trafficking and put a bounty on President Nicolás Maduro, Minister of Industry and National Production for Venezuela Tareck El Aissami, Minister of Defence Vladimir Padrino López, and President of the National Constituent Assembly Diosdado Cabello Rondón, among others. On that same day, the government announced a COVID-19 survey and screening plan using Sistema Patria as its basis. The plan, focused on house-to-house visits of those who are the most vulnerable to the disease, is an effective mechanism in the prevention and early detection of new cases. At the same time, it creates employment for healthcare workers in the midst of an economic crisis. The plan was developed by Venezuelan and Cuban medical teams who worked closely in their outreach with the various organisations of the people such as communal councils, the Local Committees for Supply and Production, health committees, and the United Socialist Party of Venezuela. Venezuela has carried out 929,599 tests to diagnose cases of COVID-19, equivalent to 30,987 tests per million inhabitants.
On 24 March, President Maduro reiterated the importance of taking preventative measures against the virus and tightened the lockdown in the Capital Region. This announcement came in light of seven new detected cases of COVID-19, bringing the country’s total at that time to ninety-one cases. This government response required at least the bolstering of three kinds of institutions: 1) Forty-six hospitals dedicated to COVID-19 patients; 2) comprehensive diagnostic centres, which were established in 2005 as local health clinics as a project of the Venezuelan and Cuban governments; 3) private health centres. Based on the latest science, the government circulated epidemiological and clinical protocols. Medications such as the Cuban anti-viral drug Interferon Alpha 2B and hydroxychloroquine were introduced to assist in the treatment of infected patients, even in private medical centres. Twelve thousand medical and nursing students were mobilised to assist in the treatment of the patients.
Venezuelans – familiar with the harsh conditions imposed on them by the sanctions – had already built relief institutions and political resilience. One such important institution is the Local Committees for Supply and Production (CLAP), which were created in 2016 as a method to deliver food to at least seven million households who were otherwise in danger of hunger. The point of the system is not only to meet the basic nutritional needs of the people, but also to strengthen local community organisations, since these are the bodies that are in touch with the people and that deliver food. Each CLAP box has similar supplies (flour, grains, rice, milk, oil, and canned meat); while the market price of the goods in the box is roughly $11, the cost to the public is less than a penny.
The CLAP programme has been under targeted attack by the United States government, which has sought to sanction overseas suppliers of food products that enter the CLAP relief boxes. This has not deterred the Venezuelan government, which – despite manifold problems – remains committed to the relief of the people. In 2016, Aristóbulo Istúriz, vice president of Venezuela, said that the programme is a ‘political instrument to defend the revolution’; this attitude remains intact. On 19 March, the government created a supplementary plan for CLAP, using the programme as a way to enhance relief at a time of the lockdown.
On 24 March, the government further extended the CLAP programme, and – despite the economic uncertainty posed by the sanctions – its distribution is guaranteed until at least August 2020. There has been a long-term plan to move from the import of food – including what goes in the CLAP boxes – to becoming more self-sufficient in food production. The government announced further investment to strengthen the Centralised Public Procurement Plan, which manages state purchases of social goods, and it encouraged the creation of ways to bring food from the countryside into cities. Since schools are closed, the School Feeding Plan, which feeds a large percentage of Venezuela’s children, has now been transformed into part of an emergency plan; drawing on a bedrock of public action, food that is cooked in community kitchens is being distributed to the students’ homes. The People to People Socialist Plan of Production, Distribution and Consumption enhances this School Feeding Plan with fruits and vegetables from productive communes and a participatory and pedagogical methodology of work. The city of Caracas has established a home delivery programme, ‘I Buy from Home’, with regulated prices of subsidised food and hired workers whose daily income had vanished as delivery persons.
A range of policies was announced on 23 March to secure the already fragile economy. Using the Sistema Patria, the government provided cash assistance to the vulnerable and to small and medium businesses directly in order for them to continue paying their workers. The government suspended lease and rent payments and prohibited evictions. It called upon real estate associations to find a way to manage the long-term crisis of insolvency. All principal and interest payments on loans were suspended for six months, and fines and interest on fines were also abolished. The government ordered banks to reclassify the measurement of credit in this period in order to protect people’s credit histories. Since communications are central – especially during the quarantine – the government prohibited the suspension of cable television services and telephone services (including the Internet) for six months. To enable the import of key goods to sustain the country, the government offered tax exemptions and invested in strategic sectors such as food production and distribution, pharmaceutical production and distribution, and the production of hygiene and sanitary equipment and goods.
In addition to such measures by the state, a key part of the Venezuelan response has been the centrality of public action. The theory of the Bolivarian Revolution is to decentralise institutional power into people power, to build institutions of the people that self-manage localities and that collectivise production. Crucial to carrying out this process are the communes, their communal councils, and the CLAP committees, as well as people’s movements. Women play a central role in the leadership of these entities as part of the Social Missions; it is women who cook every single day, who work preparing infusions and making masks, and who provide assistance to families who do not have the means to school their children at home.
The response to the pandemic is met not only by the state, but by these decentralised bodies, which are highly motivated and political. As the hybrid war against Venezuela deepens, the people’s participation not only provides vital support to counteract the impact crisis, but also strengthens their own determination to defend their Bolivarian Revolution against the attack on the currency, hyperinflation, and the armed aggression against the country intensifies popular resistance. The reaction to the pandemic – both by the state and through organised public action – has weaved relief efforts to meet people’s immediate material needs together with the political fortitude and resilience required to resist the US-led hybrid war.
Over the first six weeks of the lockdown, roughly 49,628 people returned to Venezuela, mainly from Colombia and Brazil. After being tested at the borders, they went into mandatory quarantine in government-run centres. Despite these thorough measures, many of the COVID-19 cases are imported – 77.8% of the thirty-four cases of COVID-19 identified between 9 and 27 May alone were brought in from outside of the country.
Knowing these risks, the government sent planes to Santiago (Chile), Lima (Peru), and Quito (Ecuador) to bring Venezuelans home at no cost, regardless of their political affiliations, and despite the additional obstacles to managing the crisis and accessing adequate medical supplies that are posed by US sanctions. Venezuela has faced hostility from the governments of Colombia, Peru, Ecuador, and Brazil, but this has not impacted how the government of Venezuela helped Venezuelans who migrated to those countries. Furthermore, when the Colombian Ministry of Health said that its only machine to diagnose COVID-19 had broken, President Maduro offered to send two machines, which had come from China, to Colombia – despite the fact that Colombia houses anti-Venezuelan military forces on the border and has consistently acted as a ‘doormat’ for US intervention in the country. The Venezuelan government tried to coordinate this offer through the Pan-American Health Organisation, but the offer was rejected by Colombia.
Venezuela and Cuba have been brought closer together by the US attack on both countries and by their joint commitment to socialism. The response to COVID-19 was therefore very closely coordinated by the two states. The Cuban government sent 10,000 doses of Interferon Alpha 2B; its creator – Dr. Luis Herrera – visited Venezuela on 16 March and praised the Venezuelan decision to impose quarantine as an effective way to break the chain of infection. The day before, a team of 130 Cuban doctors arrived to support the efforts to combat coronavirus in the country. This team joined the Cuban Medical Mission that has been in Venezuela since 2003 (its members rotate every two years). On 23 March, a medical team arrived from the People’s Republic of China to offer assistance, and China – along with Russia – sent medical equipment, medicines, diagnostic tests, reagents, protective lenses, biosafety suits, and air purifiers for health centres, and an air bridge was established between Venezuela and China to facilitate imports of essential goods.
In May, Iran sent five oil tankers with fuel to Venezuela with the intention of providing relief to the Venezuelan people, thereby breaking the US blockade of Venezuela’s ports. These tankers entered Venezuela with a broad message of peaceful solidarity between peoples.
![]()
A los médicos cubanos (‘To the Cuban Doctors’), Venezuela, 2020.
Miguel Guerra/Utopix
Kerala
On 18 January, KK Shailaja, Kerala’s health minister in the Left Democratic Front (LDF) government of this Indian state of 35 million, convened a meeting to discuss what was going on in Wuhan, China. Wuhan had not yet gone into lockdown, but Shailaja was aware that there were students from Kerala in Wuhan, and that when they returned, there would be a possibility of the coronavirus being imported into the state. On 22 January, the health department sent an alert to all hospitals and district authorities about the need to prepare for the virus. On 24 January, Kerala set up a state-level control room; by 28 January, control rooms had been set up in all of the districts. Isolation facilities were also set up in all of the districts, and eighteen committees were established and preventive measures were set in motion.
The first case of coronavirus in Kerala, a medical student who had been in Wuhan, was detected on 30 January; soon, two more tested positive, and by 3 February more than 2,200 people who returned to Kerala from coronavirus-hit regions had been placed under quarantine. The vigilance exercised by the state proved effective: all three patients fully recovered within a few days, and there were no cases of secondary spread. The number of people under quarantine soon decreased.
But late in February, as the coronavirus spread to more countries, the influx of people into Kerala from coronavirus-hit regions intensified. Several people – initially those coming from Italy, and later those coming from the Persian Gulf region – tested positive for COVID-19. Others who came into contact with them also contracted the disease. This was the second wave of COVID-19 infections in the state. Throughout the subsequent weeks, Kerala continued to screen passengers who came into the state not just by air, but also by road at twenty-four border checkpoints, and by train – an arduous task given the sheer number of passengers.
Kerala carried out extensive contact tracing, using route maps that contain the details of the places visited by infected persons. The people who were present at those locations during the time when the infected persons visited were asked to contact the health department. The route maps have been widely circulated through social media and through GoK Direct, the Government of Kerala’s mobile phone app. Elected representatives from Local Self Government Institutions and community health workers helped carry out contact tracing. The formula was clear: ‘trace, quarantine, test, isolate, treat’, as Chief Minister Pinarayi Vijayan – who is also a Polit Bureau member of the Communist Party of India (Marxist) – would later state.
Those who come from abroad or from other states are placed under quarantine, either at designated quarantine centres or at home. Those who have come into primary and secondary contact with infected persons are under home quarantine. Health department officials visit or call regularly to check whether isolation protocols are being followed at home. Those who do not have enough facilities at home for effective quarantining are lodged in government-run quarantine centres, and anyone who develops symptoms associated with COVID-19 is hospitalised. Testing and treatment are free and available to everyone in the state.
When COVID-19 started being reported in the state, Health Minister KK Shailaja held daily press conferences to inform the public about the latest updates, the measures being taken to combat the virus, and the measures that must be taken by the public. From 10 March onwards, Chief Minister Pinarayi Vijayan started to give daily press conferences, as the efforts to contain the pandemic now involved the work of several departments. More COVID-19 test centres and COVID-19 care centres have been set up in all districts, and 276 doctors and 321 junior health inspectors have been newly appointed.
The government has taken steps to manufacture masks and sanitiser in light of the increased demand, rather than leaving the problem to be played out in the free market. The public sector has taken the lead in producing more medicines, hand sanitiser, and gloves. Kudumbashree, a massive government-backed collective of neighbourhood groups of 4.5 million women (roughly one-fourth of the population of women in the state), started making masks. Activists of the left-wing Democratic Youth Federation of India (DYFI) and the Kerala Sastra Sahitya Parishad (‘The Kerala Forum for Science Literature’ or KSSP, Kerala’s biggest people’s science movement) pitched in by making hand sanitiser.
The government launched the Break The Chain campaign to encourage people to adopt the practices necessary to prevent COVID-19 infection. Government employees’ organisations set up hand sanitiser kiosks in front of government offices. DYFI set up hand washing facilities in 25,000 locations across the state, and call centres for people who needed help. Preparedness, utmost vigilance, strict adherence to protocol, and transparency have been crucial in Kerala’s battle against COVID-19.
By late March, when the rest of India awoke to the reality of the pandemic, Kerala had already moved towards an in-depth plan to alleviate the economic hardship of the people. By 12 March, it had announced the closure of educational institutions and soon began to deliver food at home for children who would have otherwise been in childcare centres. Rather than impose a blanket lockdown with no thought as to how families might eat, stay in their homes, or comply with the policies being rolled out – as done by India’s central government – Kerala’s state government gradually put restrictions into place, taking care to provide the people with the conditions to follow them. On 19 March, the Chief Minister announced a relief package of Rs. 200 billion. The package included advance payment of social welfare pensions, free food grains to everyone for a month, additional funding of Rs. 5 billion for public healthcare, and relaxation of utility bill and tax payment deadlines.
The state implemented a lockdown from 24 March onwards. India’s central government implemented a country-wide lockdown from the next day onwards. In the subsequent weeks, Kerala’s state government distributed food grains for free to all families in the state. Cooked food is being provided to the elderly who live alone, the disabled, those who cannot cook for themselves due to illness, and the extremely poor. Ward-level committees of Local Self Government Institutions (LSGIs) – panchayats in villages, municipalities in towns, and municipal corporations in larger cities – are doing this work with the help of volunteers. Community kitchens have been set up by the LSGIs, and volunteers deliver cooked food from these kitchens to the homes of those in need. Members of the left-wing unions of LSGI employees, such as the Kerala Municipal and Corporation Staff Union (KMCSU), constitute a majority of those who are volunteering their services at the community kitchens. The government has also distributed grocery kits containing seventeen essential items to all families for free.
Anticipating the possibility of supply chains being disrupted due to the lockdown, the state government took steps to ensure that paddy, the staple crop of the region, is harvested without interruption. Measures were also taken to ensure the procurement of rice, vegetables, and several other crops.
Right at the outset, the Government of Kerala recognised that the accommodation facilities for migrant workers from other Indian states were often inadequate to ensure physical distancing. Therefore, state-run relief camps were set up for the workers and medical check-ups were arranged. Food, masks, soap, and hand sanitiser were made available to the workers. As of 20 April, 19,902 camps had been opened for migrant workers in Kerala, with 353,000 workers staying in the camps – the highest number of such camps in the country.
Kerala has many welfare fund boards for workers of various sectors, which provide social security benefits by pooling contributions by workers and their employers into welfare funds. All workers in sectors with welfare fund boards are being provided financial assistance through the boards. Workers who are not part of any welfare fund board are being given Rs. 1,000 each.
The scale of voluntary work that is underway is massive. Apart from voluntary work by government employees, trade union members, youth activists, and student activists, work by the Social Volunteer Force of youth set up by the government has also been a crucial part of the relief efforts. As of 23 June, 346,306 youth had registered as volunteers who are working to identify those who need assistance, deliver food and essential items, provide emergency assistance at homes, help with the operation of call centres and control rooms, deliver materials to relief camps, communicate alerts, and provide assistance at hospitals.
Kerala’s efforts to contain the second wave of COVID-19 infections were successful – by 8 May, the number of active COVID-19 cases in the state had come down to just sixteen. But a third wave of infections began soon after. This was because, as part of the easing of the lockdown in India, the severe restrictions on inter-state travel and on the arrival of international flights which were in place began to be relaxed from the first week of May onwards. Hundreds of thousands of Keralites living abroad and in other Indian states, faced with rising COVID-19 infections and deaths, unsafe conditions, a lack of medical attention, and even job losses in many cases, scrambled to get back to their home state. The state government adopted the stand that it is committed to bring back all Keralites who wanted to return to the state. More than 315,000 people returned to Kerala from other states and abroad between 4 May and 23 June. Since most of those who return come from regions with very high numbers of COVID-19 cases, this led to an increase in the number of infections in Kerala.
As of 23 June, the number of active COVID-19 cases in Kerala stood at 1,620, and the number of deaths at 22. Out of all the cases reported in the state from 4 May to 23 June, 90.7%f were reported among those who came from abroad or other states. A total of 150,196 people were under observation at this point – 147,990 at home or at quarantine centres, and 2,206 at hospitals. Restrictions are being relaxed in a calibrated manner, but there is no room for complacency. Awareness campaigns are continuing, norms about physical distancing are in place, large gatherings are not allowed, and the use of face masks in public is compulsory. The state government continues to hold regular press conferences and provide daily updates for the public.
The efforts of the LDF government are rooted in a comprehensive approach to ensure the welfare of all citizens. This is an approach which recognises the importance of the public healthcare system, as well as other social and economic determinants of health and well-being. It recognises that hunger and homelessness would be serious impediments to health. The LDF government’s policy measures amid COVID-19 aim to address all of these issues in order to provide relief to the people.
The objective is to reach every single person in need. As of 9 June, 116,328 volunteers had been deployed to identify those who need assistance so that no one falls through the cracks. The government’s strategy has been to mobilise its entire state machinery, including the public sector and LSGIs, along with the collective energies of the state’s powerful mass and class organisations, collectives, and cooperatives, and the zeal of Kerala’s citizens for voluntary action. This is a strategy of total mobilisation that integrates the work of the state machinery with the work of the general public, with those mobilised by mass and class organisations playing a key role.
All of this has been made possible as a result of public action in the state. Right from the time when the first communist ministry was elected in 1957, Kerala has invested in public education and public healthcare. Communist-led governments have taken the lead in implementing land reforms that broke feudal landlordism, greatly improved the living standards of the peasantry and agricultural workers, and increased the bargaining power of the workers. The working-class movement has played a crucial role in Kerala’s wages being the highest in the country, and has served as the most important factor behind the state having the most wide-ranging social security measures for workers, through the welfare fund boards.
The Left has long championed democratic decentralisation. The biggest effort in that direction was the People’s Plan Campaign, initiated by the LDF government in 1996. The LSGIs were greatly strengthened by the People’s Plan Campaign, which led to much higher devolution of funds and powers to the local bodies. This has significantly expanded the capacity of the LSGIs to intervene effectively in times of need, and now they are spearheading the relief efforts in the state. Kudumbashree was also initiated by the LDF government in 1998 and strengthened in the subsequent tenures of the LDF.
Public healthcare in Kerala has received its biggest boost over the tenure of the present LDF government, which came to power in 2016. This is in large part due to the Aardram Mission, an ambitious programme launched in 2017 to upgrade the state’s public healthcare facilities. Kerala has long had the best system of primary healthcare in the country, centred on Primary Health Centres (PHCs). The present LDF government has carried forward and significantly expanded upon this legacy. Now according to official rankings, the top twelve PHCs in India are in Kerala. As part of the Aardram Mission, all PHCs are being upgraded to Family Health Centres (FHCs) with extended timings (FHCs have outpatient services from morning to evening, compared to morning to noon in PHCs) and more doctors. Facilities in all government hospitals have improved greatly. This is what has enabled the healthcare system to stand up to the challenge posed by COVID-19. At the same time, efforts by the central government led by the far-right Bharatiya Janata Party (BJP) to push privatisation in the healthcare sector have been resisted by the LDF government of Kerala. In February of this year, the central government proposed that the district hospitals in Indian states should be privatised, and Kerala flatly refused.
The Very Best of Human Possibilities
CoronaShock reveals a deep divide between capitalist and socialist countries. This divide can be best understood, as we have shown, along four axes:
Socialism
- Science
- Public sector
- Public action
- Internationalism
Capitalism
- Hallucination
- For-profit sector
- Atomisation and paralysis of the population
- Jingoism and racism
There are, of course, exceptions to these reactions among the capitalist states. Several states in East Asia – such as Japan and South Korea – as well as Australia and New Zealand had been prepared by the SARS outbreak of 2003, and they did not destroy their public health infrastructure in the decades that followed; based on the experience of SARS, they did not scoff at the WHO reports.
By and large, however, it is the socialist states that have confronted the virus with resolve and intelligence; this is even though they face the brunt of US imperialism and an increasingly aggressive hybrid war (especially in the case of Cuba and Venezuela). These societies and their states have acted with determination and tenacity to break the chain of the pandemic and to avoid creating individual and social trauma and an economic desert for their peoples. Capitalism is unable to confront a disaster that it has in many ways created; socialism, on the other hand, brings out the very best of human possibilities.
Cover image adapted from People’s Medical Publishing House, China, 1977. Credit: Tricontinental